
Automação Industrial com Segurança e Eficiência
Especialistas em adequação de máquinas conforme a NR12 para indústrias em busca de produtividade, conformidade legal, e modernização de equipamentos. Saiba mais!
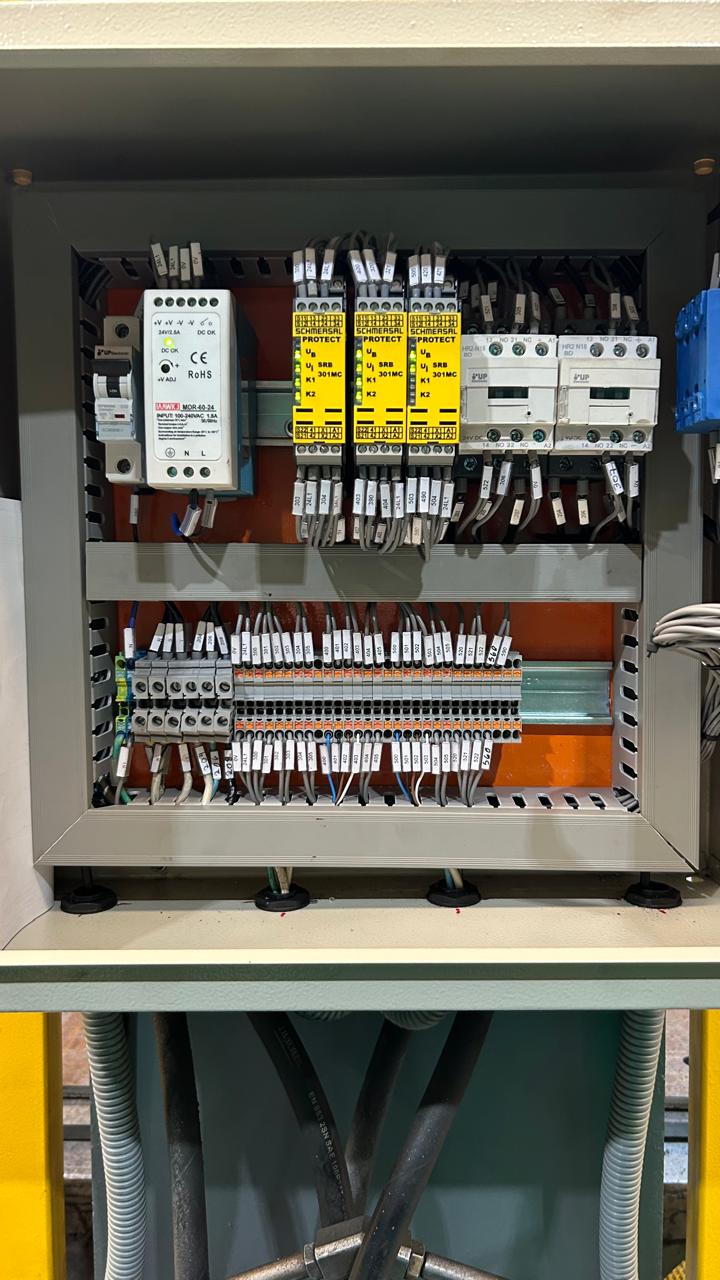
Fotos


Automação Industrial com Segurança e Eficiência
Especialistas em adequação de máquinas conforme a NR12 para indústrias em busca de produtividade, conformidade legal, e modernização de equipamentos. Saiba mais!
Nossos Serviços
Especializados em automação industrial, oferecemos soluções adaptadas às suas necessidades.

Adequação NR12
Conformidade de máquinas com as normas de segurança vigentes.

Painéis Elétricos
Projetos e montagem de painéis para automação eficiente.

Automação Industrial
Soluções completas que otimizam processos e aumentam a produtividade.

Consultoria Técnica
Suporte especializado para atender suas demandas específicas.

Líderes em Automação Industrial
Somos especialistas em automação industrial, dedicados à segurança e adequação máquinas conforme a NR12. Nossa missão é fornecer soluções para indústrias que buscam aumentar a produtividade, garantir conformidade legal, reduzir riscos operacionais e modernizar equipamentos. Oferecemos serviços abrangentes, desde adequação de máquinas à consultoria técnica especializada. Comprometemo-nos a entregar segurança, eficiência e resultados para sua empresa.
Por que nos escolher?
Conheça os motivos para optar pela MB12 automação industrial.
Expertise em NR12
Especialistas em adequação de máquinas conforme normas de segurança.
Soluções Personalizadas
Atendemos às necessidades específicas de cada indústria.
Suporte Técnico Dedicado
Apoio contínuo para garantir eficiência e segurança.
Depoimentos
Veja o que nossos clientes têm a dizer sobre os serviços da MB12 Automação Industrial
Marina Silva
A MB12 proporcionou segurança e eficiência em nossos processos industriais, superando nossas expectativas.
Pedro Oliveira
Com a automação da MB12, conseguimos cumprir as normas de segurança e aumentar nossa produtividade.
Camila Santos
O suporte técnico da MB12 foi fundamental para modernizarmos nossos equipamentos e evitar riscos operacionais.
Perguntas Frequentes
Esclareça suas dúvidas sobre nossos serviços de automação industrial.
O que é a NR12?
A NR12 é uma norma regulamentadora que estabelece diretrizes de segurança para máquinas e equipamentos, visando proteger os trabalhadores e garantir um ambiente seguro.
Quais indústrias podem se beneficiar dos serviços da MB12?
Atuamos em diversas indústrias que buscam melhorias na segurança, produtividade e eficiência de máquinas, independente do setor de atuação.
Como funciona a adequação de máquinas conforme a NR12?
Realizamos uma análise detalhada das máquinas, identificando adequações necessárias para garantir a conformidade com a NR12 e a segurança operacional.
Vocês oferecem suporte técnico após a instalação das soluções?
Sim, oferecemos consultoria e suporte técnico especializado para garantir o funcionamento adequado e contínuo das soluções implementadas.
Quanto tempo leva para adequar uma máquina?
O tempo necessário varia conforme a complexidade da maquinaria e as adequações necessárias. Após uma avaliação técnica, podemos fornecer um prazo estimado.
Como posso agendar uma visita técnica?
Você pode agendar uma visita técnica entrando em contato conosco pelo telefone 51992845510 ou pelo e-mail atendimento@mb12.com.br.
Perguntas Frequentes
Esclareça suas dúvidas sobre nossos serviços de automação industrial.
O que é a NR12?
A NR12 é uma norma regulamentadora que estabelece diretrizes de segurança para máquinas e equipamentos, visando proteger os trabalhadores e garantir um ambiente seguro.
Quais indústrias podem se beneficiar dos serviços da MB12?
Atuamos em diversas indústrias que buscam melhorias na segurança, produtividade e eficiência de máquinas, independente do setor de atuação.
Como funciona a adequação de máquinas conforme a NR12?
Realizamos uma análise detalhada das máquinas, identificando adequações necessárias para garantir a conformidade com a NR12 e a segurança operacional.
Vocês oferecem suporte técnico após a instalação das soluções?
Sim, oferecemos consultoria e suporte técnico especializado para garantir o funcionamento adequado e contínuo das soluções implementadas.
Quanto tempo leva para adequar uma máquina?
O tempo necessário varia conforme a complexidade da maquinaria e as adequações necessárias. Após uma avaliação técnica, podemos fornecer um prazo estimado.
Como posso agendar uma visita técnica?
Você pode agendar uma visita técnica entrando em contato conosco pelo telefone 51992845510 ou pelo e-mail atendimento@mb12.com.br.